Ages (3-5)
On the Ages 0-3 page, we discussed the first two steps of obtaining an Autism Spectrum Disorder diagnosis – Developmental Monitoring and Developmental Screening. If developmental monitoring and screening have found some reason to pursue further evaluation, there are some things you should know.
Step 3 - Evaluation
- There is currently no medical test, based on biology, that can definitively evaluate and diagnose ASD.
- Evaluations will include taking a developmental history, observation, interaction, and clinical judgment by a qualified professional. Because of the methods used in the evaluation, there is some level of subjectivity to the outcome. If you disagree with the outcome, it is ok to seek a second (or third) opinion.
The Utah Autism Initiative has compiled a list of Autism Evaluation Providers including contact information and insurance accepted. This might be a good place to start to find a qualified professional to conduct your child’s evaluation.
Some tools used by providers to evaluate for ASD include the Autism Diagnostic Observation Schedule (ADOS-2) and the Autism Diagnostic Interview-Revised (ADI-R). The ADOS-2 consists of a series of tasks requiring interaction between the evaluator and your child. Behaviors are observed and categorized, scored, and then analyzed to determine where they fit on a standardized scale which then leads to a diagnosis. The ADI-R is a parent interview that focuses on reciprocal social interaction, communication and language, and patterns of behavior.
Why did you seek an evaluation?
Step 4 - Diagnosis
The point at which Social Communication Impairment and Restricted Interests/Repetitive Behavior intersect is where ASD lies. The diagnosis of Autism Spectrum Disorder comes from the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM 5). To see the specific diagnostic criteria, click here.
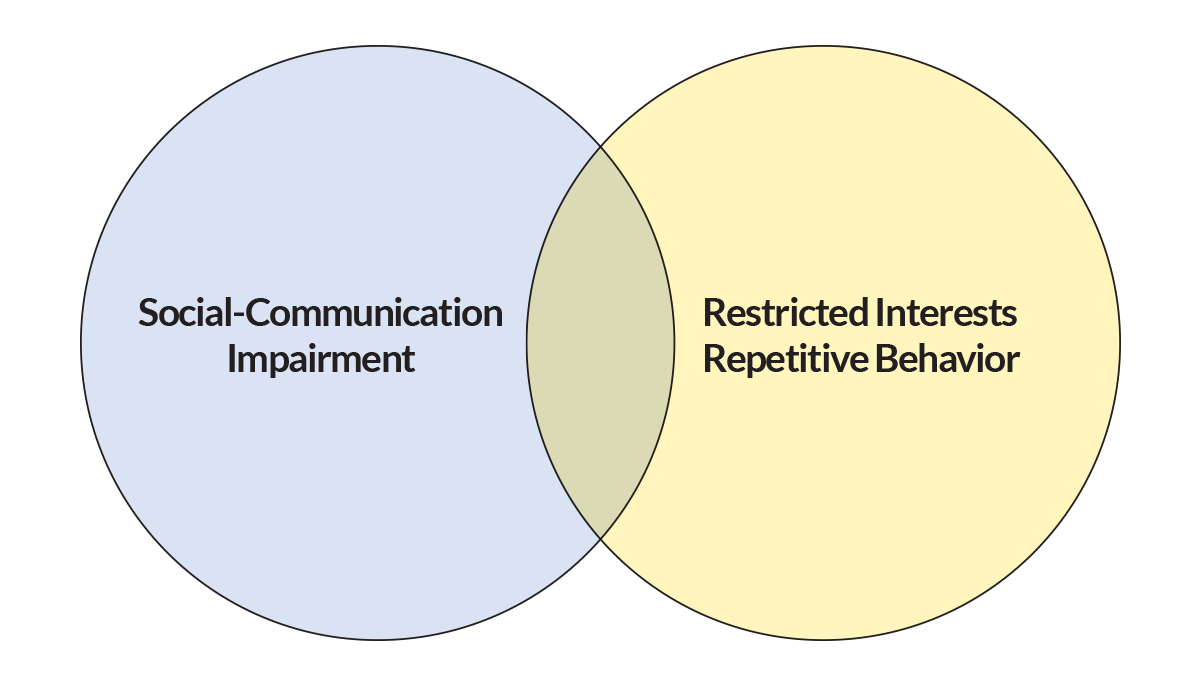
To receive a diagnosis of Autism Spectrum Disorder, the child must demonstrate persistent deficits in Social Communication and the presence of Restricted Interests and Repetitive Behaviors in multiple contexts. They must present themselves from a young age.
The child must have Social Communication Impairment in all three of the following areas:
- Social-Emotional Reciprocity
- Lack of back-and-forth conversations
- Difficulty sharing enjoyment and interests
- Difficulty with empathy and perspective-taking
- Non-Verbal Behavior
- Difficulty with eye gaze, gestures, and body language
- Lack of facial expression or over-exaggerated expressions
- Developing Relationships
- Lack of interest in peers
- Difficulty developing or maintaining friendships
- Challenges with cooperative or imaginative play with others
The child must also demonstrate the presence of Restricted Interests and Repetitive Behaviors in at least two of the following areas:
- Stereotypical repetitive behavior – hand flapping, spinning, pacing, repeating words or scripts
- Rigid, inflexible behavior – rituals, distress with transitions or changes in routines
- Abnormal obsessive interests – in objects, activities, topics, or parts of objects
- Sensory differences – needing sensory input (spinning, rolling up in a blanket, etc.) or avoiding/disliking sensory input (covering ears, shutting eyes, hating strong smells, etc.)
The symptoms must cause significant impairment to the child and not be better explained by an intellectual disability or global developmental disability.
Reference: Seattle Children’s Hospital, Autism 101 Presentation: https://www.seattlechildrens.org/health-safety/keeping-kids-healthy/development/autism-101/
Be aware that, according to studies, males and females differ when looking at the diagnosis of ASD. Males are diagnosed at a rate that is four times higher than females, and females tend to be diagnosed later than males. This may be because females seem to have fewer communication deficits and better coping strategies. Females may display different types of restrictive or repetitive behaviors that are more socially acceptable as compared to males, such as playing dress-up with dolls for extended amounts of time. As a parent, if you think that your daughter may have autism, you may want to find an evaluator who is familiar with diagnosing females so they know what to look for. For more information on the differences between the presentation of Autism in males and females, you can continue to read here.
Reference: PsychCentral https://psychcentral.com/pro/child-therapist/2019/11/comparison-of-males-and-females-with-asd-gender-differences-in-people-with-autism-spectrum-disorder
As part of the diagnosis, the person conducting the evaluation will attempt to identify the severity of the impact of the symptoms:
- Level 1 – Requiring support
- Level 2 – Requiring substantial support
- Level 3 – Requiring very substantial support
The evaluator will also specify if the diagnosis comes with or without an accompanying intellectual impairment (if that can be determined – common in about 30% of those with autism) and with or without an accompanying language impairment (25-35% of those with autism are considered minimally or non-verbal). For example, a child may be diagnosed with ASD Level 1 without intellectual or language impairment, or ASD Level 2 without intellectual but with language impairment, among other possibilities.
| NOTE: The levels and accompanying impairment assigned can be subjective and especially hard to determine in very young children. While the ASD diagnosis may not change, the levels and accompanying impairments can be different as the child grows. |
The Utah Autism Initiative, along with the Autism Council of Utah, has developed this aid to assist parents in the evaluation and diagnosis process. It can help you to know what to expect as well as what questions to ask during the process.
Intervention Options
The number and types of interventions for autism are many and varied. Autism is a spectrum disorder so there is a wide spectrum of options to access to help treat the symptoms. There is currently no “cure” for autism but many interventions have been proven to improve abilities and skills. Interventions can maximize the ability of the individual to function as independently as possible so that they no longer meet the criteria for the diagnosis of Autism. Some autism interventions may be covered by health insurance. To determine your plan’s coverage, read the member benefits or talk with a plan administrator. This article has information on laws regarding insurance requirements for treating autism in Utah.
The Centers for Disease Control breaks out autism interventions into four categories:
- Behavior and Communication Approaches
- Dietary Approaches
- Medication
- Complementary and Alternative Medicine (CAM)
- Behavior and Communication Approaches
- Dietary Approaches
- Complementary and Alternative Medicine Treatments
- Medication
Behavior and Communication Approaches
According to reports by the American Academy of Pediatrics and the National Research Council, behavior and communication approaches that help children with ASD are those that provide structure, direction, and organization for the child in addition to family participation.
Some of the common interventions used include:
- Applied Behavior Analysis (ABA)
- Assistive Technology
- Cognitive Behavior Therapy
- Functional Behavior Assessment (FBA)
- Occupational Therapy
- Peer Therapy
- Social Skills Training
- Speech Therapy
Click here for a list of specific programs and additional resources
Dietary Approaches
Dietary treatments are based on the idea that there is a brain-gut connection, and that some food allergies or lack of vitamins and minerals cause or exacerbate symptoms of ASD. Even food additives like certain food dyes have been said to affect individuals with ASD. Recent research has demonstrated a greater prevalence of gastrointestinal (GI) symptoms in children with ASD as compared to their typically developing peers. To resolve these issues, a nutritional therapist can provide parents with information to create lifelong healthy habits in children experiencing gut- and brain-connected diagnoses.
Functional medicine and health coaches believe that the brain will heal if you treat the body. A Functional Medicine Doctor investigates the root cause of inflammation and illness in the body and provides a nutritional plan to implement a more holistic approach to identifying and addressing behaviors and sensory eating patterns commonly seen in children with autism. To find qualified nutrition-based providers, click here.
Be Prepared! Your child’s bowel movement, commonly known as poop, is often a topic of discussion among autism parents because we get it. We get that some kids will play with it and smear it. Some withhold it and get constipated, even impacted. Some constantly have diarrhea. We understand you may have many doctor visits and discussions around poop. You may find yourself tracking how often, what it looks like, and more. Know now that it may be a part of your life and vocabulary for many years to come.
Complementary and Alternative Medicine Treatments
To relieve the symptoms of ASD, some parents and healthcare professionals use treatments that are outside of what is typically recommended by pediatricians. These treatments are known as complementary and alternative medicine (CAM) treatments. CAM treatments refer to products or services that are used in addition to or instead of traditional medicine.
Many of these treatments have not been studied for effectiveness. Before starting such a treatment, talk to your child’s doctor. The FDA has information about potentially dangerous treatments here.
Some common examples of CAM treatments include, but are not limited to:
- Use of essential oils and/or aromatherapy to manage mood or behavior
- Massage therapy – use of massage to apply deep pressure or lessen the need for sensory input
- Emotion work/energy work/foot zoning – focus on managing emotions, balancing the body systems, helping to heal the body using pressure points in the feet
- Cannabidiol (CBD) oil – used to alleviate stress and anxiety as well as help with seizures
- Chelation – a process designed to remove heavy metals from the body
- Music therapy – addresses the social, emotional, physical, and intellectual needs of individuals using activities such as listening, drumming, moving, singing, etc.
- Chiropractic care – there are many modalities of chiropractic care but all seek to heal the body through proper alignment
- Herbology- use of herbal medicine to attempt to help with the symptoms of autism
- Acupuncture – using very fine needles placed strategically in the body to attempt to lessen the symptoms of autism
- Hippotherapy – specialized horse-back riding which may improve balance, strength, and motor coordination among other things
Integrative medicine is another holistic approach to health and wellness. Visit the Mayo Clinic for further information about integrative medicine. An all-inclusive list of functional and integrative medicine professionals can be found here.
Medication
There are no medications that can cure ASD or treat the core symptoms. However, some medications can help many people with ASD function better. For example, medication might help with co-existing conditions such as:
- High energy and/or Inability to focus – Attention-Deficit/Hyperactivity Disorder (ADHD)
- Anxiety
- Depression
- Seizures
- Obsessive-Compulsive Disorder (OCD)
- Sleep disorders
- Gastrointestinal issues
Medications do not affect all children the same. Be sure to work with a healthcare professional who has experience in treating children with ASD and monitor your child while taking medication to ensure any negative side effects do not outweigh the benefits.
To learn more about medication and ASD, please visit the National Institute of Child Health and Human Development.
These documents can help you decide if medication is right for you/your child: ATN/AIR-P Medication Decision Aid, and ATN/AIR-P Autism and Medication: Safe and Careful Use.
A Word About Communication
The American Speech-Language-Hearing Association says everyone has a right to effective communication, whether through spoken words, or augmentative and alternative communication, also called AAC. AAC is a broad category that includes sign language, gestures, pictures, written words, and electronic devices. Find a way that works for your child to express their wants and needs. It may be through words or signs, or through low-tech picture icons put on a strip. Or it could be through an app or speech-generating device. IDEA requires that public schools provide assistive technology devices and services to students with IEPs so be prepared to discuss your child’s communication needs. The school district’s Assistive Technology (AT) team can do an evaluation and assessment to help you find a method that works best for your child. Click here to find the AT specialist for your district. Click here for more information about speech therapy interventions.

Get Organized
An important step is to get organized with a good calendar system to track appointments and therapies. This will become invaluable as you juggle various aspects of your child’s needs and the rest of the parts of your life. You will be your child’s lifetime advocate and primary care manager. Find a way that works for you to keep all of the information you will be receiving organized and accessible so that you can find it when you need it. It is helpful to have a way to log calls, emails, and texts, and a tracking system for the things you need to do. Your system may be paper-based, electronic, or a combination of both, whatever is best for you and your family. A Care Notebook, designed to be a more comprehensive organization tool, is mentioned on the Ages 0-3 page.
Other on-the-go tools you might find useful to take to medical and therapy appointments, to keep in your car or on your fridge for emergencies, or to provide to other caregivers include:
- Getting to know me document, (click here for Spanish)
- Emergency contact document, (click here for Spanish)
- Health Care Information
”One of the issues that we want to look at, an important issue, is what happens to you (the family) when you hear about the diagnosis.
Dr. Douglas Goldsmith
Home and Community
Now What?
Parent Responses to Concerns about Autism
What happens to us? When we have this sweet little child whom we love so much, and someone tells us that there is something “different” about them? Even though we were in search of answers, it is still a shock to have those concerns validated. After the shock passes, we are left thinking, “What do we do now?”.
What happened to you when you were told your child needed further evaluation or were given a diagnosis?
- Did you have a therapist or healthcare provider ask how they could help you?
- Did you go out and find support from somewhere: a grandparent, close friend, clergyman, family member, or another parent?
- Did you want to talk about it at all?
- Did you find comfort in the literature you were given, or on the internet?
There is a wide range of responses and there is no right or wrong way to deal with the news of the diagnosis. The following are some common reactions of family members to the news their child has ASD:
There is a wide range of responses and there is no right or wrong way to deal with the news of the diagnosis. The following are some common reactions of family members to the news their child has ASD:
Connecting Parents with Parent Peer Supports
It can be helpful at this stage to find other parents who are going through, or who have gone through, what you are going through. There is a poem likening finding out your child has autism to someone who planned a trip to Italy and instead finds themselves in Holland. It was written by Emily Perl Kingsley in 1987 and is titled, “Welcome to Holland.” Some parents really relate to it and others find it highly flawed, but the fact that it is still making the rounds more than 30 years after it was written shows that parents want a way to express what it is like to have a child who is different from what they may have anticipated. We want to connect with other parents who “get it.” The parent-to-parent connection is so important, we have compiled a list of organizations and groups that provide support to families on the Utah Parent Center website. This list [link to Connecting With Peer Supports pdf] is not exhaustive but it is a good place to get started making connections with parents and others who understand your circumstances.
Resources
- Childmind – Sharing an Autism Diagnosis with Family and Friends https://childmind.org/article/sharing-an-autism-diagnosis-with-family-and-friends/
”I received very harsh judgment from my parents and in-laws about how I parent my son. But people that have never spent a significant amount of time with a person with autism can’t give you good advice. They honestly do not know what they’re talking about. It’s taken me a few years to learn how to let people’s judgment roll off my back and be ok with how I do things.
Childcare Considerations
Good childcare is important to many families. Having a child with autism brings additional challenges to finding childcare that works for your family. For example, your child may not yet be potty trained and may not be eligible for some programs as a result. (Many parents we surveyed mentioned potty training difficulties.) Or your child may exhibit challenging behaviors that create problems for the childcare facility and may result in being asked not to return.
While these scenarios or others like them may happen, there are still many childcare options available and good childcare is possible. It just may take a little more work and collaboration.
The Office of Child Care (OCC) is part of the Department of Workforce Services here in Utah and its mission is to provide accessible, affordable, and quality childcare for Utah children. Their website offers many tips and resources to parents who are looking for childcare.
Care About Childcare here in Utah has a searchable feature to look for providers trained in, or willing to be trained in, ASDs, as well as a list of parenting resources.
The Utah Parent Center has developed a handout with ideas for childcare for parents of children with significant disabilities.
The Center for Inclusive Childcare has created a handout, particularly for parents whose children have special needs with questions to ask providers to find the right one for their family.
For those who would like some help managing challenging behaviors, Autism Speaks has a Childcare Provider Guide with information specifically for childcare providers.
Raising Children, a parenting website from Australia also provides a description of, and responses to, challenging behavior. Sesame Street in Communities has a page on Autism that offers explanations, activities, and more for parents and caregivers to use to promote understanding.
Collaborative Team-Building
The saying “It takes a village to raise a child” is especially true when raising a child with autism. You will want to build a team of people, your village, to help you. This may include your friends and family, childcare providers, healthcare professionals, therapists, teachers, and more. Each will bring their own perspective to the table and can help you support your child. Working together, you can build a bright future for your child.
Some tips to help you in working as a team are:
- Communicate clearly
- Show respect and gratitude for all team members
- Keep your child as the focus
Be certain you clearly communicate with members of the team and make sure that they know how to communicate best with you. Communication can help break down barriers that keep people from working effectively together. It helps, for example, if the speech therapist, occupational therapist, preschool teacher, healthcare professional, and autism treatment therapist are all aware of what each other is working on and can support each other. As the common connector, you can ensure that information is communicated to everyone and keep them informed of progress.
Respect everyone on the team and value their perspective and input. Realize that they bring skills and abilities that you may not have. It’s important to express gratitude for what everyone is doing on behalf of your child and family. They have chosen to help you with your child and are vested in the outcome. It is important to keep an open mind and try new approaches before they are dismissed. Remember, however, that while others may have your child’s best interests at heart, you are the parent and have the right to respectfully refuse or disagree with a suggestion or recommendation if you do not feel it is right for your child or family. Trust that “gut” feeling, but also be receptive to feedback and suggestions from the team.
Always keep your child at the center of focus for everyone on the team. This can help when there are disagreements on goals or procedures. Focusing on the child reminds everyone who is important. Whatever is best for the child should be the outcome, not what best fits someone’s schedule or idea of what is the right course of action.
Building and collaborating with your “village” can help you provide your child with a lifetime of support.
”Educate teachers and caregivers about your child's abilities. Seek out professionals who are supportive and create a care team.
Typical Peer Interactions
Interaction with peers is important for all children but especially so for children with Autism Spectrum Disorder (ASD). This is because playing with typical peers helps those with ASD to develop problem-solving, language, and social skills as they interact and see appropriate behavior being modeled by others. In fact, studies have found that interaction, play, and conversation improved over time with preschoolers with ASD, showing better interaction and social skills which leads to children being more included with their peers. As a parent, you can help facilitate peer interactions for your child.
- Natural opportunities for interaction with typically-developing peers occur in childcare settings. It may be helpful to find out if there are any children from childcare that might enjoy a structured play date with your child doing something that both children enjoy.
- Trips to the neighborhood playground are also opportunities for peer interaction. Talk with other parents who are at the playground and see if any would be interested in participating in an organized playgroup or in meeting on a regular basis.
- Community classes provide opportunities to connect with other children who may have a similar interest to your child. Dance, arts and crafts, martial arts, sports, etc. are all opportunities to provide interaction with typical peers.
- Faith-based groups often have opportunities for parents and children to gather together informally and provide peer support for both you and your child.
The Utah Parent Center offers lists of recreational activities available throughout the state including camps and classes, summer programs, and all-ability playgrounds.
More about peer interventions as a therapeutic treatment is discussed in the section, Working With Professionals and Systems.
A word here about “stims” or self-stimulating behavior. Stims, or stimming, refers to repetitive movements or sounds and is often engaged in by children with autism. In truth, we all have stress-reducing activities we engage in – tapping fingers or toes, biting your lip, etc. – that could be considered stims but for those with autism, stims can become excessive and cause problems.
The same thing is true of special interests. Everyone has things they enjoy but autistic children may have interests that are very specialized and may be intense in level of enjoyment and dedication to them. In the past, therapists may have encouraged the extinction of stims and only allowed an ASD child to engage with a preferred interest after completing a task as a reward, and only for a few minutes. But current studies are showing the best course of action is to ignore the stims and to encourage special interests.
Some stims are socially inappropriate, like sucking on fingers or putting your hand in your pants. Those need to be reshaped or replaced or only allowed to happen in private. And some interests and stims can interfere with daily living. In that case, they may need to be limited to specific times and places.
If your child engages in stims while playing with other children, it may impact how the other children view your child. The same is true of unusual interests your child may have. Other children may not be interested in the same things and it can impact friendships. Try to find ways to educate other children about stims to help them see it as a normal coping mechanism, and help your child expand their interests by engaging them with other children.
Education and Employment
Entering the Education System
There are a few different ways your child can begin receiving education services, even if they are not old enough to go to kindergarten.
- If they receive early intervention services, the early intervention team will help you through the transition to special education preschool services, if eligible, when they turn 3. See the Utah Parent Center website for helpful resources.
- If they receive a diagnosis after turning 3, they may be referred to a special education preschool by a pediatrician, healthcare provider, or other specialists for an educational evaluation.
- Parents can also call their local school district and request an evaluation for preschool services; this can be done even before or without receiving an official diagnosis elsewhere. Screenings and educational evaluations provided by the school district are free of charge to families.
Note: An evaluation for special education services is not the same as an evaluation to receive a diagnosis. An education evaluation is used to determine if the child meets the qualifications in one of several categories to be eligible for special education. A qualified clinician can conduct an evaluation for an autism diagnosis but the child may still need to be evaluated by an education specialist to determine eligibility for school services. A medical diagnosis does not guarantee eligibility for special education services.
If found eligible for special education, a team including the parents and school personnel will gather to create an Individualized Education Program or IEP. The IEP documents what the student’s needs are, what goals the student will work to meet, and what services will be provided to help the student reach their goals. It is a written commitment from the Local Educational Agency (LEA) (generally local school or district personnel) of resources that will be allocated to help the student succeed. It is also used to ensure compliance by the school with state and federal laws pertaining to special education.
Some children whose level of need does not meet the requirements for special education may be eligible for services under Section 504 of the Rehabilitation Act of 1973, which also protects the rights of persons with disabilities. A Section 504 plan is developed by a team that includes the parents and can provide the student with accommodations or services that are needed for accessing the school environment and curriculum. More about Section 504 plans can be found on the Utah Parent Center website.
Note: There are a lot of terms and acronyms used in special education that may be new to you. For a list of acronyms and what they stand for, click here<.
For a glossary of terms, click here.
To understand the special education process in more detail, including evaluation, eligibility, and IEPs, click here.